Is Xanax Linked to Dementia?
While the exact cause of dementia is still largely unknown to experts, there are many possible risk factors to be considered. Some of the basic things that one can do to minimize the risk of developing dementia include:
- Eating a healthy diet
- Exercising regularly
- Getting adequate sleep
- Keeping the mind engaged
In today’s fast paced and busy world, it’s not easy to achieve all of the above. Some people then choose to take medications that can help them achieve them. Xanax, for example, is a drug that many people in the United States take on a regular basis. Experts have now found that long term use of medications such as Xanax could possibly increase the risk of developing dementia.
QUICK LINKS - TOPICS COVERED:
- WHAT IS XANAX?
- XANAX AND RISK OF DEMENTIA
- XANAX PRESCRIBED FOR DEMENTIA
- SHOULD MY LOVED ONE TAKE XANAX?
What is Xanax?
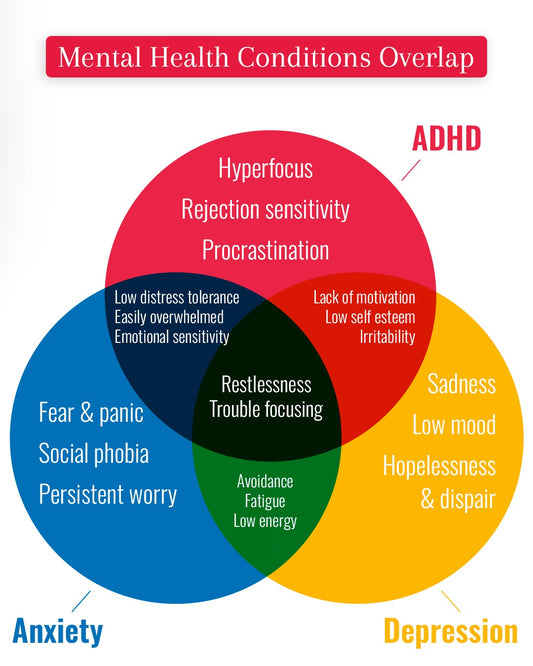
Alprazolam, better known as Xanax, is a drug that is used to treat anxiety and panic disorders. It belongs to a class of medications called benzodiazepines. The drug works by influencing neurotransmitters in the central nervous system to produce a calming effect. There are several types of benzodiazepines available in the market. Some of the most commonly prescribed brands include:
- Xanax
- Klonopin
- Valium
- Ativan
Xanax and Risk of Dementia
Researchers have looked into the use of Xanax and other benzodiazepines and the risk of dementia. While taken in the short term, the medication is considered safe. However, when is taken like a regular daily pill for over several months, patients run the risk of becoming addicted and experiencing cognitive decline such as confusion, clouded thinking, and memory lapses.
A few studies have looked into the connection between the use benzodiazepines such as Xanax and dementia patients. In one study[1], researchers from France and Canada linked benzodiazepine use to an increased risk of being diagnosed with Alzheimer's disease. In the study, the researchers looked at the drug prescriptions during the five to six years preceding the Alzheimer's diagnosis. They determined that the greater people's cumulative dose of benzodiazepines, the higher their risk.
People who had taken a benzodiazepine for three consecutive months or less had about the same dementia risk as those who had never taken one. But those who had taken a benzodiazepine for three to six months had a 32% greater risk of developing Alzheimer's, and those taking one for more than six months had an 84% greater risk than those who hadn't taken one.
The type of drug taken also mattered. People who were on a long-acting benzodiazepine like diazepam (Valium) or flurazepam (Dalmane) were at greater risk than those on a short-acting one like triazolam (Halcion), lorazepam (Ativan), alprazolam (Xanax), or temazepam (Restoril).
Xanax Prescribed for Dementia
As a person’s dementia progresses, caregivers—and even the patient themselves—may find that their symptoms become increasingly difficult and stressful to manage. In such instances, they tend to look for solutions that would help them to manage those symptoms better. While Xanax in itself isn’t an FDA approved medication for dementia, many doctors often prescribe it ‘off-label’ to treat some of the symptoms such as agitation, anxiety, and insomnia.
Should My Loved One Take Xanax?
It is understandable that you’d want to help your loved one manage their symptoms as best as possible. Since there is still no cure for dementia, medications that help manage and possibly delay symptoms are the next best thing. However, in the case of drugs such as benzodiazepines, you should weigh the pros and cons thoroughly before coming to a decision.
Although it is still rather common practice for doctors to prescribe Xanax and similar drugs for dementia patients, many other medical professionals warn against doing so, especially in older people. In 2012, the American Geriatrics Society[2] added benzodiazepines to their list of inappropriate medications for treating insomnia, agitation, or delirium. That decision was made primarily because common side-effects of benzodiazepines—confusion and clouded thinking—often have disastrous consequences, including falls, fractures, and auto accidents.
Even short-acting benzodiazepines pack a bigger punch in older people. As the body’s metabolism slows with age, drugs take longer to clear. And because benzodiazepines are stored in body fat, they can continue to produce effects days after people stop taking them.
Because of this, in 2013 the American Geriatrics Society recommended to not use benzodiazepines, such as Xanax, or other sedative-hypnotics in older adults as first choice for insomnia, agitation or delirium[3]. Medications such as these should be used carefully, at low doses, and as a last resort. Instead, do consider non-drug management approaches[4] or even a combination of approaches first.
[1] https://www.health.harvard.edu/blog/benzodiazepine-use-may-raise-risk-alzheimers-disease-201409107397
[2] https://www.health.harvard.edu/blog/benzodiazepine-use-may-raise-risk-alzheimers-disease-201409107397
[3] https://betterhealthwhileaging.net/choosing-wisely-healthcare-aging-adults-part-1/
[4] https://betterhealthwhileaging.net/how-to-manage-difficult-alzheimers-behaviors-without-drugs/