Care Arrangement: Geriatric Psychiatric Facility
When a loved one suffering from a degenerative brain disease like dementia starts to experience changes in their behavior, us caregivers are hopeful that it might be a temporary change, or that it was just this one time and might never happen again.
Days and weeks pass and those "once in a blue moon" episodes where you or your loved ones safety might be in question become more regular and eventually something snaps, it's too much and you need help for your loved one.
Geriatric Psychiatric Facilities are there to focus in on how to stabilize your loved one by assessing their current medications and identifying what other options your loved one has to ensure they, yourself and everyone around them is safe and happy.
Read on for more details on this great resource available when you might need it the most!
QUICK LINKS - TOPICS COVERED:
- WHAT IS A GERIATRIC PSYCHIATRIC FACILITY?
- THE NUMBERS BEHIND GERIATRIC PSYCH FACILITIES
- RATIO OF PATIENTS TO CAREGIVERS
- WHEN DOES SOMEONE GO TO A GERIATRIC PSYCH UNIT?
- SERVICES AT GERIATRIC PSYCH FACILITY
- ADMISSION PROCESS
- DISCHARGE PLANNING
- COMMON ISSUES
WHAT IS A GERIATRIC PSYCHIATRIC FACILITY?
The term Geriatric Psychiatry Unit was introduced in 1984 by Dr. Norman White MD and it translates to a hospital-based geriatric psychiatry program.
With increases in life expectancy, particularly in the developed countries, there has been an increase in the number of people showing what is called a “Geriatric Syndrome”. Geriatric Syndrome is a term often used to refer to common health conditions in elderly adults that do not fit into a distinct organ-based disease and usually have multi-factorial causes. These conditions may include cognitive impairment, delirium, malnutrition, incontinence, imbalance, gait disorders, pressure ulcers, sleep disorders, fatigue, and dizziness, among others. Therefore, as the population ages, these types of care arrangements become increasingly important and needed.
Sometimes it becomes extremely difficult for a caretaker to provide and to stand up to the needs of an elderly person, especially with dementia. This is magnified at times of crisis, which is another reason for the existence of Geriatric Psychiatry Units.
A Geriatric Psychiatry Unit is a specialized unit that focuses on the older population—people above 55 or 65 (depending on the institution) years of age—and it is designed to evaluate and treat a patient with or without concurrent medical issues. They usually admit people 24h per day, for a short duration (usually about 1-2 weeks). These hospital units provide a team of professionals that may include psychiatrists, internists, psychologists, nurses, social workers, mental health therapists, nutritionists, occupational and physical therapists.
THE NUMBERS BEHIND GERIATRIC PSYCH FACILITIES
RATIO OF PATIENTS TO CAREGIVERS
In most cases, a Geriatric Psychiatric Unit has between 10 and 30 beds and includes 1 to 2 doctors and 3 to 5 nurses. This level of doctor or nurse to patient ratio is deemed to be of a good level where it allows for patients to receive adequate care and attention from the staff.
WHEN DOES SOMEONE GO TO A GERIATRIC PSYCH UNIT?
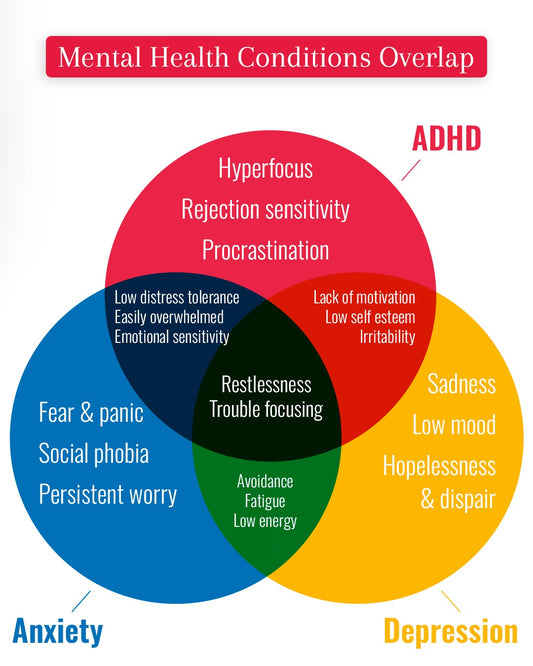
- Seem depressed
- Seem anxious
- Seem aggressive
- Talk about committing suicide
- Behave in a way that interferes with the caregivers’ ability to care for them
SERVICES AT GERIATRIC PSYCH FACILITY
- On-going medication consultation by a licensed and board certified psychiatrist.
- Coordination of services by a treatment team of professionals led by the attending psychiatrist.
- Discharge planning by a social worker.
- Group sessions by social workers, occupational therapists, registered nurses, recreational therapists and other professionals.
- Tests and examinations to determine the needed care and treatments.
ADMISSION PROCESS
You can also research on the web for more information. Below is a helpful site that lists the Geriatric Psychiatric Units across the United States: Link.
Why Must A Patient Go To The ER to be Admitted?
The admission to a Geriatric Psychiatric Ward implies that a patient is suffering through some type of acute episode. Thus, the ER is the first place to take the patient in a situation like this. This way, it is easier for relevant healthcare professionals to evaluate whether or not the patient needs to be admitted to the Geriatric Psychiatry Unit.
In the ER (which can take a couple of hours), the staff will check for UTI's or other easily treatable conditions that may be causing the episode before making the decision to refer the person to the Psychiatric unit. This trip to the ER can be distressful for families and the patient.
Handling the Situation during Admission
As mentioned above, admittance into a Geriatric Psychiatric Unit is through the ER, where the initial process is started. However, it is not easy to keep a dementia patient calm in a place like the emergency room. The surroundings are new and different. It can be very noise and overwhelming, which can cause the patient’s confusion to increase dramatically. Therefore, it is even more important to do as much as possible to keep them as calm as possible. The following actions by a caregiver may be able to help with the calm down process:
- Have atleast one person that they know with them at all times
- Holding the person’s hand
- Talking softly and with a low voice
- Keeping calm
- Asking for help, if necessary
There are some hospitals for example, in Canada, where a different approach is used. The patients are given some of the tools that will be used on them in an ER. They are shown images of nurses in masks and scrubs to try and see beyond the disease. It is a process that has had excellent results in maintaining calmness with people in the ER.
What Is The Admittance Process?
When a patient arrives, the unit’s lead staff (nurses and/or doctors) will evaluate the condition of the patient. After a thorough examination, if the patient meets the necessary criteria, they are admitted to the Geriatric Psychiatric Unit after meeting with a social worker that assists the family with completing the necessary documentation.
What Can The Patient Take With Them Into The Ward?
Normally, there isn’t a need to take many personal items when being admitted to the ward. It is also highly likely that the hospital will not allow the patient to have anything else with them besides their clothes. Except for clothing and personal care items, all other services are provided. This includes nutrition, laundry, and medication administration.
Does Insurance Pay?
Insurance is complicated and sometimes frustrating these days. Medicare and many insurance companies cover certain services. However, even with large providers, full coverage may not be available for the program advised for your loved one. Therefore, it is extremely important to research and investigate the cost of different programs in different facilities ahead of time if possible. That way, not only will you avoid being caught off guard, but also be prepared for situations when you have to ‘pay out of your pocket’.
Typically Medicare Part A (Hospital Insurance) covers the majority of the cost. It includes mental health care services that one gets in a hospital that requires admittance as an inpatient. These services can be obtained either from a general hospital or a psychiatric hospital that only cares for people with mental health conditions. At a psychiatric hospital, Part A only pays for up to 190 days of inpatient psychiatric hospital services during a patient’s lifetime.
Medicare does not cover the following items:
- Private nursing duties
- Phone or television in the patient’s room
- Personal care items
- Private room—unless medically necessary
Other than that, most facilities also tend to offer payment plans so that the cost can be managed without causing stress on you or your loved one’s finances. It should be noted that if the finances for treatment is poorly planned and/or managed, it can have some serious consequences. For example you or your loved one’s assets may have to be taken away in order to pay for the necessary care. This is why it is vital to be as well informed about the costs of Geriatric Psychiatric Units as early in the process as possible.
DISCHARGE PLANNING
- Patient and/or substitute decision maker
- Prime nurse
- Psychiatrist
- Social Worker
- Family Physician or another allied health clinician, as required
If the patient is being transferred back to their home to live independently, often a social worker and occupational therapist may assist this process by doing a home assessment to ensure that the patient has the necessary skills and resources to care for their self and live independently.
In cases where the patient is returning to a long-term care home, staff from the facility and associated geriatric psychiatry outreach team is also invited to the discharge meeting to ensure that all necessary support systems are set up in advance.
Sometimes when the hospital discharges patients, the care facilities may not take them back. The abandonment of many low-income patients is a nationwide problem. The reason for this tend involve complicated issues between care facilities that complain of low Medicaid payments, hospitals that require people to find another facility to take in the patient, and frail elders and their families. It should be noted that according to federal law, skilled-nursing facilities are required to give residents 30 days’ notice if they to discharge a patient.
Care facilities may have various reasons for not taking back patients. Some of which are:
- The residents require extreme care or have behavioral issues, such as emotional agitation or abusive outbursts. In these cases, facilities usually send the residents to hospitals with behavior units to get assessed or have their medications regulated
- Professional training is available to help employees handle these situations, but the cost is not covered by the already low Medicaid reimbursement
- Cost of care is higher than the state Medicaid rate
COMMON ISSUES
Incident Reports and Filing Complaints
A geriatric psychiatry unit must report any serious incidents using the complaint intake system and location designated by the department within 24 hours following its occurrence. An incident report shall be submitted in written form to the inpatient psychiatric service provider's chief executive officer or designee within twenty-four hours of discovery of the incident.
An incident is defined as any event that poses a danger to the health and safety of patients and/or staff and visitors of the hospital, and is not consistent with routine care of persons served or routine operation of the hospital.
The inpatient psychiatric service provider shall develop an incident reporting system to include a mechanism for the review and analysis of all reportable incidents such that clinical and administrative activities are undertaken to identify, evaluate, and reduce risk to patients, staff, and visitors. The inpatient psychiatric service provider will also maintain an ongoing log of its reportable incidents for departmental review.
Anyone who has knowledge of any instances of abuse or neglect, or alleged or suspected abuse or neglect, or of an alleged crime which would constitute a felony, must report the incident immediately. The inpatient psychiatric service provider shall notify the patient's parent, guardian or custodian, if applicable, within twenty-four hours of discovery of a reportable incident, and document such notification. The notification may be made by phone, mailing, faxing or e-mailing a copy of the incident form, or other means according to inpatient psychiatric service provider policy and procedures.
When notification does not include sending a copy of the incident form, the inpatient psychiatric service provider must inform the parent, guardian or custodian of their right to receive a copy, and forward a copy within twenty-four hours of receiving a request for a copy.
Serious incidents that must be reported to the department include the following:
- Any accidental or unanticipated death of a patient not directly related to the natural course of the patient's underlying medical condition.
- Any serious injury to a patient that requires medical treatment.
- Any rape, assault, any battery on a resident, or any abuse, neglect, or exploitation of a patient.
- What happened?
- To whom did it happen?
- When did it happen?
- Where did it happen?
- Who did the abuse?
- Who was responsible for the neglect?